Borderline Personality Disorder
Specialized, compassionate treatment for lasting stability and integration.
If you or someone you love has been diagnosed with Borderline Personality Disorder, you may have encountered significant stigma—from clinicians, from loved ones, perhaps even from yourself. BPD is one of the most misunderstood and unfairly maligned diagnoses in mental health. It’s also one of the most treatable personality disorders, with evidence-based therapies that lead to genuine, lasting change.
I specialize in the treatment of BPD. I approach this work with deep respect for the suffering involved and confidence in the possibility of recovery. People with BPD can and do get better. They develop stable identities, form lasting relationships, regulate their emotions, and build lives worth living.
Understanding Borderline Personality Disorder
Borderline Personality Disorder is characterized by pervasive instability: in relationships, in self-image, in emotions, and in behavior. This instability isn’t willful or manipulative—it reflects genuine difficulties in the basic psychological capacities most people take for granted: knowing who you are, managing intense feelings, and maintaining a stable sense of others.
At the core of BPD is a profound sensitivity and a history that made that sensitivity unmanageable. Most people with BPD experienced early environments that were invalidating, traumatic, or both. They learned that their feelings were too much, that relationships were unreliable, that they couldn’t trust their own perceptions. These adaptations made sense in context but create immense suffering in adult life.
BPD is not a character flaw. It’s not an insult to be hurled by frustrated clinicians or exhausted family members. It’s a serious condition that causes real suffering—and it responds to appropriate treatment.
- Intense, unstable relationships
- Unstable self-image or sense of identity
- Impulsive behaviors that cause harm
- Recurrent suicidal behavior or self-harm
- Emotional instability and reactivity
- Chronic feelings of emptiness
- Intense, inappropriate anger
- Paranoia or dissociation under stress
- Fear of abandonment
What It’s Like to Live with BPD
If you have BPD, you likely know intimately what it feels like to:
In Relationships
- Feel terrified of being abandoned, even when evidence says otherwise
- Idealize someone one moment and feel betrayed by them the next
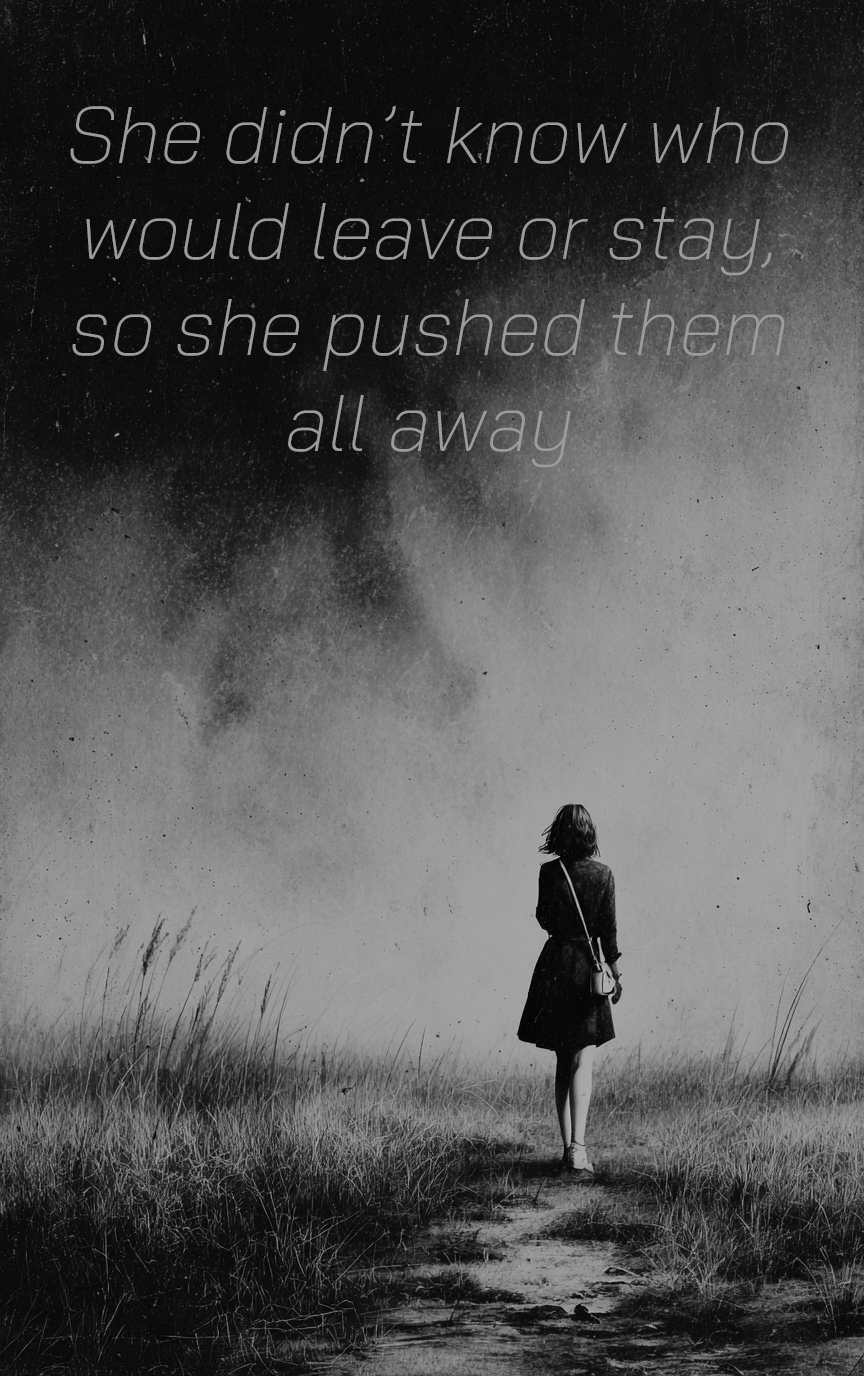
- Push people away when you desperately want them close
- Feel that you’re always too much or never enough
- Have relationships that feel incredibly intense but don’t last
In Yourself
- Not know who you really are, or feel like it keeps changing
- Feel empty inside, as if something essential is missing
- Experience emotions so intense they feel unbearable
- Turn to self-harm, substances, or other behaviors to cope
- Have thoughts of suicide as a way to escape the pain
“The paradox of BPD is that the behaviors that push others away are often attempts to prevent the abandonment that feels unbearable. Understanding this paradox is the first step toward change.”
Evidence-Based Treatment
I offer two specialized, evidence-based treatments for BPD, both grounded in psychodynamic understanding and supported by strong research evidence.
Mentalization-Based Treatment (MBT)
Mentalization is the capacity to understand behavior—your own and others’—in terms of underlying mental states: thoughts, feelings, wishes, and beliefs. People with BPD often struggle to mentalize, especially under stress. When mentalization fails, you lose the ability to understand why you or others are behaving in certain ways, leading to misinterpretation, impulsive reactions, and relational chaos.
MBT focuses on developing and strengthening this capacity. In therapy, we slow down to examine what was happening in your mind during difficult moments: What were you feeling? What did you imagine the other person was thinking? What assumptions did you make? Through this careful, curious examination, you gradually build the ability to pause, reflect, and respond rather than react.
Key Features of MBT:
- Focus on present moments and current relationships
- Emphasis on curiosity over certainty
- Attention to what happens in the therapeutic relationship
- Development of reflective capacity
- Reducing black-and-white thinking
Transference-Focused Psychotherapy (TFP)
TFP, developed by Otto Kernberg and colleagues, works directly with the patterns that emerge in the therapeutic relationship. The “transference” refers to how you unconsciously repeat relationship patterns from your past in the present, including with your therapist. These patterns contain crucial information about your internal world.
In TFP, we pay close attention to what happens between us: when you feel I’ve failed you, when you’re certain I’m judging you, when you feel intensely attached or want to flee. By examining these experiences together, we can understand the internal “objects”—the internalized relationships—that organize your experience. This work leads to integration: a more stable sense of self and others that can hold complexity and contradiction.
Key Features of TFP:
- Clear treatment frame and contract
- Focus on what happens in session, in the moment
- Analysis of splitting and other defenses
- Integration of split-off parts of self and other
- Development of identity consolidation
The Path to Stability and Integration
Treatment for BPD is not about becoming a different person. It’s about developing the internal capacities that were disrupted or never fully developed.
Stabilization
The first phase focuses on safety: reducing self-harm, managing crises, and establishing a stable treatment frame. We work on developing basic coping capacities and building a therapeutic relationship that can withstand the storms ahead.
Pattern Recognition
As treatment progresses, we begin to identify the recurring patterns that cause you suffering: the expectations you bring to relationships, the defenses you use against unbearable affect, the ways your past shows up in your present. This is slow, careful work.
Working Through
Change happens through working through: encountering the same patterns again and again, understanding them more deeply each time, and gradually developing new ways of responding. The therapeutic relationship becomes a laboratory for this work.
Integration
The goal is integration: developing a stable, coherent sense of self; the ability to hold complex, ambivalent feelings about yourself and others; emotional regulation that doesn’t require destructive action; and the capacity for genuine, lasting intimacy.
What Recovery Looks Like
Stable Identity
You develop a consistent sense of who you are that doesn’t shift dramatically based on who you’re with or how you feel. You know your values, your preferences, your history. You experience yourself as continuous over time.
Emotional Regulation
Emotions remain intense but become manageable. You develop the capacity to experience strong feelings without being overwhelmed by them or needing to act on them destructively. Distress tolerance increases.
Lasting Relationships
Relationships become more stable and satisfying. You can hold mixed feelings about people without splitting. Conflict doesn’t mean abandonment. Intimacy becomes possible without losing yourself.
Studies consistently show that most people with BPD improve significantly over time, especially with appropriate treatment. The McLean Study of Adult Development found that 85% of people with BPD achieved remission within 10 years, and that once remission was achieved, relapse was uncommon. This is a treatable condition. Recovery is not just possible—it’s expected with proper care.
For Family Members and Partners
Loving someone with BPD can be exhausting, confusing, and heartbreaking. You may feel like you’re walking on eggshells, unable to predict what will trigger a crisis. You may be the target of intense anger one moment and desperate need the next. You may feel manipulated, even when you intellectually understand that’s not quite what’s happening.
A few things are worth knowing:
- The behavior isn’t willful. What looks like manipulation is usually a desperate attempt to manage unbearable feelings or prevent feared abandonment.
- Your loved one isn’t choosing to suffer. They’re caught in patterns that developed as survival strategies and are now causing immense pain.
- Treatment works. With the right therapy, real change is possible. But recovery takes time, and there will be setbacks.
- You need support too. Caring for someone with BPD takes a toll. Your own therapy, support groups, or education can help you cope and set appropriate boundaries.
- Boundaries aren’t abandonment. Clear limits, consistently held, are actually stabilizing for people with BPD, even when they initially react badly.
I’m available for consultation with family members who want to better understand their loved one’s condition and their own responses to it.
Is This Treatment Right for You?
Specialized treatment for BPD requires commitment. It’s intensive work—typically meeting once or twice weekly for one to several years. It involves confronting painful patterns and tolerating difficult emotions within the therapeutic relationship. It requires showing up consistently, even when part of you wants to flee.
This treatment may be right for you if:
- You’ve been diagnosed with BPD or suspect it might fit
- Your relationships consistently follow painful, destructive patterns
- You struggle with a stable sense of identity
- Emotional dysregulation significantly impacts your life
- You’re tired of treatments that haven’t addressed the core issues
- You’re ready to commit to intensive, longer-term work
- You want lasting change, not just crisis management
If you’re uncertain whether this approach is right for you, a consultation can help clarify. I’ll give you an honest assessment of whether I think I can help and, if not, point you toward alternatives that might be a better fit.
Common Questions
What treatments do you use for BPD?
I primarily use Mentalization-Based Treatment (MBT) and Transference-Focused Psychotherapy (TFP), both evidence-based treatments specifically developed for BPD. These approaches focus on understanding emotional experiences, improving relationship patterns, and developing a more stable sense of self. Treatment is tailored to each individual’s needs.
How long does BPD treatment typically take?
BPD treatment is typically long-term, often 2-4 years, though meaningful improvement often begins much sooner. The length reflects the complexity of personality-level change—we’re not just addressing symptoms but fundamentally shifting longstanding patterns. Many clients notice significant improvements in emotional regulation and relationships within the first year.
What’s the difference between MBT and TFP?
Both are effective evidence-based treatments for BPD. MBT focuses on improving your ability to understand mental states—your own and others’—which helps regulate emotions and navigate relationships. TFP works more directly with the patterns that emerge in the therapy relationship itself to understand and change problematic relationship dynamics. I often integrate elements of both approaches.
Can BPD be treated effectively?
Yes, absolutely. Research consistently shows that specialized treatments like MBT and TFP lead to significant improvement for most people with BPD. Many individuals no longer meet diagnostic criteria after treatment, and most experience meaningful reduction in symptoms like emotional instability, self-harm, and relationship difficulties.
Is BPD the same as being “difficult” or “manipulative”?
No. BPD is a serious mental health condition characterized by difficulties with emotion regulation, unstable relationships, and an unclear sense of identity—often resulting from early adverse experiences. Behaviors that may seem “manipulative” are usually desperate attempts to manage overwhelming emotions or prevent feared abandonment. With proper treatment, these patterns can change significantly.
Take the First Step
Recovery from BPD is possible. Schedule a consultation to discuss whether we might work well together.